Huntington’s disease is a devastating and progressive inherited disorder that is caused by the expansion of the CAG trinucleotide sequence in the huntingtin (HTT) gene. This mutation results in abnormally long versions of the HTT protein, which progressively destroy neurons in the brain. Those affected experience a gradual loss of mental function and physical control as the disease progresses, with symptoms typically first appearing between age 30 and 50, and worsening over a 10-25 year period. At present, there is no effective treatment or cure for Huntington’s Disease, only drugs that can mask symptoms to some extent but do not slow the disease’s progression.
But recent developments give hope that this may change in the future. On December 12, Roche exercised its option on IONIS-HTTRx, triggering a $45 million license payment to IONIS for rights to the antisense drug candidate, which is under development as a potential disease-modifying treatment for Huntington’s Disease. Roche’s decision was based on positive Phase 1/2a clinical data from an international trial where the drug was administered intrathecally to 46 adult patients with early manifest Huntington’s Disease. This study showed that by binding to and inactivating the messenger RNA involved in production of the HTT protein, the mutant gene can be silenced and production of the toxic protein reduced.
Hailed by some in the scientific community as an important breakthrough, IONIS-HTTRx is the first drug to show an effect on the underlying pathology of Huntington’s Disease. However, it remains to be seen in future clinical trials whether reducing the production of the toxic mutant HTT protein will actually prevent or slow the disease, or produce other benefits for patients—despite some past animal research data suggesting it might.
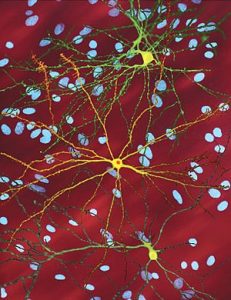
For one thing, the HTT protein is expressed ubiquitously throughout the body, although at very high levels in the brain and testes. While the exact function of the HTT protein is unknown, it appears to play a role in nerve cell function and it regularly interacts with proteins found only in the brain. IONIS-HTTRx is designed to reduce the production of all forms of the HTT protein: What will be the long-term effects of reducing total HTT protein levels?
This potential new treatment also raises other important questions. If IONIS-HTTRx proves to benefit those with Huntington’s Disease, when should treatment begin, given that the damage is progressive? And if future clinical data supports treating affected individuals early in life—well before symptoms appear—when should screening for the Huntington’s mutation begin? Should screening start in childhood or perhaps at age 18, when someone may be a bit better equipped to decide whether they want to know their status or to make important decisions about a likely life-long treatment?
And if IONIS-HTTRx does offer benefits, does success in Huntington’s Disease point to a way forward in other progressive neurological illnesses, where accumulation of toxic proteins plays a key role, like amyloid and tau in Alzheimer’s disease and synuclein in Parkinson’s disease?