 Many important basic discoveries about human biology have been made using “model organisms” — more primitive species with biological processes that have been carried down through evolution to humans. Recently, researchers at Vanderbilt University and the University of Michigan identified a protein, TRAP-alpha, in nematode worms (Caenorhabditis elegans) which appears to be key for proper insulin synthesis, folding and secretion. This protein is conserved across worms, flies and mammals, including humans, and its understanding could lead to new approaches to prevent and treat type 2 diabetes.
Many important basic discoveries about human biology have been made using “model organisms” — more primitive species with biological processes that have been carried down through evolution to humans. Recently, researchers at Vanderbilt University and the University of Michigan identified a protein, TRAP-alpha, in nematode worms (Caenorhabditis elegans) which appears to be key for proper insulin synthesis, folding and secretion. This protein is conserved across worms, flies and mammals, including humans, and its understanding could lead to new approaches to prevent and treat type 2 diabetes.
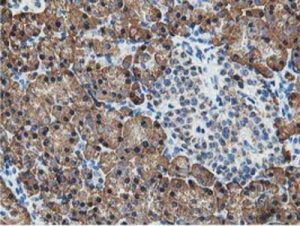
TRAP-alpha modulates the PI3K/Akt signaling pathway. Alterations in this pathway have been linked to a range of diseases, including cancer, cardiovascular disease and diabetes. TRAP-alpha is part of a complex that helps fold and move newly synthesized proteins into cells for further processing before they are secreted.The researchers discovered that deleting TRAP-alpha in the worms reduced insulin signaling. Similarly, deletion of TRAP-alpha in the pancreatic beta cells of rats led to a 90% reduction in total insulin synthesis. This was due to preproinsulin — a precursor molecule to insulin — not being properly transferred into the endoplasmic reticulum of the altered beta cells for final processing, and secretion. Instead, the unfolded protein accumulated in the beta cells and was degraded. As a result, without TRAP-alpha, insulin production was significantly impaired.
In other recent diabetes research, scientists at Weill Cornell Medicine and New York-Presbyterian showed that the protein adipsin, produced by subcutaneous body fat, helps shield pancreatic beta cells from destruction in type 2 diabetes.
When the researchers experimentally increased adipsin levels in mice with type 2 diabetes, they observed long-term positive effects, including lower blood sugar and higher insulin levels as well as reduced beta-cell death. They found that adipsin activates C3a, an effector of the complement system, which protects and supports beta-cell function. C3a acts by suppressing the enzyme Dusp26 which can damage and kill beta cells. When the investigators suppressed Dusp26 in the mice with type 2 diabetes, the animals exhibited healthier beta cells that were able to secrete more insulin.
These findings appear to carry over to humans. An evaluation of 5,570 participants from the Framingham Heart Study found that individuals with higher adipsin blood levels had a lower risk of developing diabetes than people with lower levels of the protein. The incidence of the disease was ~50% lower in participants with the highest adipsin levels. The research team is now investigating whether inhibiting Dusp26 production in beta cells might be a target for drug development, as a means to protect beta cells in people with type 2 diabetes and preclude their eventual need for insulin injections.