The association between Alzheimer’s disease (AD) and amyloid protein has existed since the early 1900s, when Alois Alzheimer recognized that amyloid plaque deposits, along with neurofibrillary tangles, were defining features in the brains of people who died with memory loss and dementia. In the late-1980s, researchers identified the main component of the plaques as beta-amyloid (Aβ), a small cleavage product of the larger amyloid precursor protein (APP). It thus became a predominant theory that excess or mis-processed Aβ production resulted in plaque formation, which drove AD pathology. Support for this also came from the observation that hereditary mutations in the APP gene, which resulted in easier Aβ cleavage, led to early AD onset. For those subscribing to this amyloid hypothesis, the other brain pathologies seen in AD-affected brains – neurofibrillary tangles and activated astrocytes and microglia involved in clearing dead cells and debris – were interpreted as downstream effects resulting from the amyloid deposits’ toxicity to neurons.
As a result, the search for treatments that could block amyloid plaque formation or clear such plaques from the brain, potentially slowing the progression of AD or even restoring some cognitive function, has been central for decades to much AD drug discovery. Unfortunately, until very recently, most drug candidates failed to significantly clear amyloid plaques and diminish cognitive decline. Most recently, Roche’s Aβ-targeting antibody gantenerumab, failed to slow cognitive and functional decline in people with early AD in either of two randomized, double-blind, placebo-controlled Phase 3 studies. Even Biogen and Eisai’s Aduhelm (aducanumab), which ultimately gained FDA approval in June 2021, did not significantly reduce cognitive decline in treated patients. As a result, the amyloid hypothesis began to fall out of favor.
In November 2022, however, the situation changed with the release of results from a Phase 3 trial of Eisai and Biogen’s second anti-Aβ antibody, lecanemab, that validated the importance of amyloid plaques as a therapeutic target for AD. The trial showed for the first time that targeting Aβ can both reduce amyloid plaques in the brain and produce a statistically significant slowing of cognitive and functional decline in individuals with AD. The companies received an accelerated approval for lecanemab (now branded as Leqembi), on January 6, 2023 and immediately filed for a full approval.
Additionally in November 2022, Eli Lilly announced mid-stage results from the company’s double-blind, placebo-controlled Phase 3 TRAILBLAZER-ALZ4 study of donanemab, the company’s own Aβ-targeting antibody, versus aducanumab (Adulhelm). Results at six months showed a clearance of 65.2% for donanemab versus 17% for aducanumab. The mid-stage results were not sufficient to support an accelerated approval for donanemab, which was denied by the FDA in January 2023 for lack of sufficient patients with at least 12 months exposure to the antibody therapy. According to Lilly representatives, the trial protocol allowed trial participants to wean off the drug early as a result of rapid plaque clearance, something experienced by an (as yet undisclosed) number of patients. However, Lilly expects the Phase 3 trial to complete in Q2 2023 with sufficient patients meeting the 12-month drug exposure criterion and to serve as the basis of a full approval for donanemab. We will be on the lookout for those results.
In the past several months, new evidence in favor of the theory that amyloid plaque deposition is the driving factor in Alzheimer’s disease has emerged, as well as new understanding of amyloid toxicity in the brain. For example, three different forms of Aβ have been identified, with most drug development over the past decade targeting either Aβ monomers or the fibrillar Aβ aggregates that deposit into plaques. Acumen Pharma, in contrast, is developing an antibody, designated ACU193, that selectively targets non-fibrillar oligomers of Aβ — the most toxic form of that protein, associated with nerve synapse deterioration and loss, inflammation, and other events that may lead to memory and cognitive impairment and chronic neurodegeneration. ACU193 is currently in a Phase 1 clinical safety study in patients with early-stage AD.
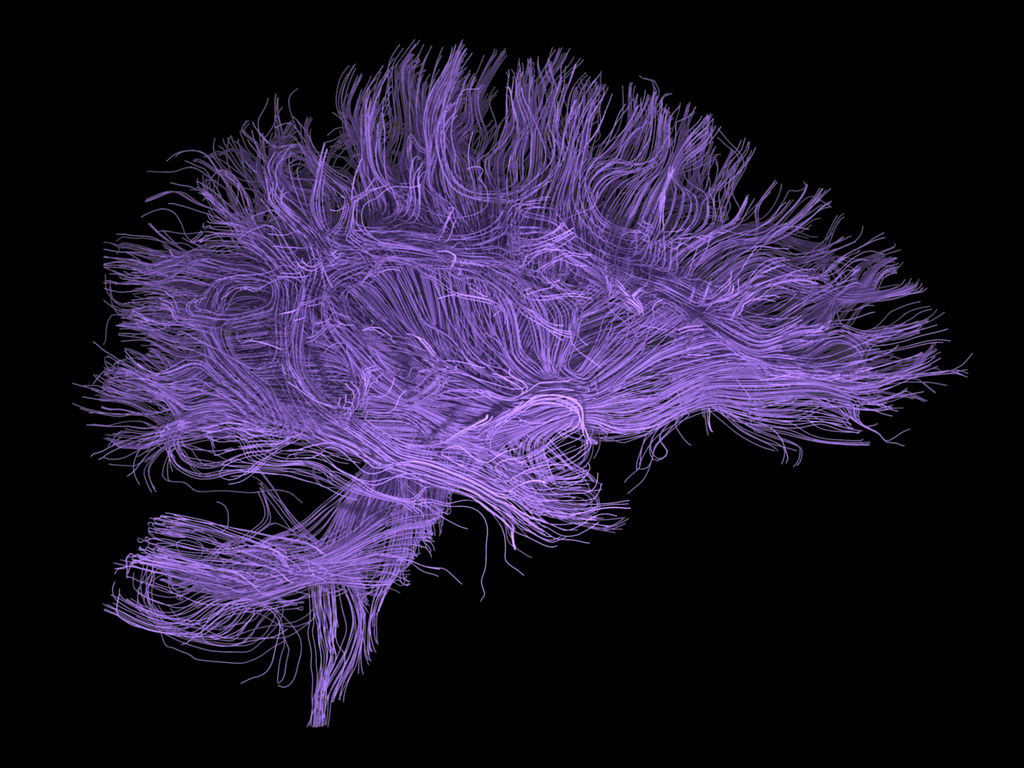
Moreover, new strategies and drug targets are being explored as potential avenues to stimulate plaque clearance. Companies such as Alector are seeking to enhance the activity of microglia cells, immune cells in the central nervous system that are involved in removing wastes from the brain, and therefore could be harnessed to remove Aβ deposits. Alector is developing two potential antibody treatments for AD based on this approach. AL002, partnered with AbbVie and currently in a Phase 2 clinical trial, targets the TREM2 receptor on myeloid cells with the goal of optimizing TREM2 signaling to improve cell survival and proliferation and activity if microglia.
Alector’s other antibody, AL044, instead targets MS4A, a gene selectively expressed in microglial cells. One MS4A variant appears to be a genetic risk factor for late-onset sporadic AD. MS4A is hypothesized to regulate multiple aspects of AD risk and progression: the rate of Aβ and Tau accumulation, the rate of cognitive decline, the rate of brain tissue loss, the rate of conversion from mild cognitive impairment to AD, and the age of onset and survival with AD. The AL044 antibody is designed to reduce AD risk associated with the MS4A gene variant by improving the recruitment and activation of microglia to counteract multiple AD disease pathologies, either as a single agent or in combination with therapies against misfolded proteins. By stimulating the brain’s immune system to counteract disease pathologies, Alector says that AL044 represents “a paradigm shift in therapies for neurodegeneration akin to immuno-oncology.” Alector began a Phase 1 clinical trial with AL002 in September 2022.
Recent research findings have also pointed to several other potential drug targets. For example, scientists at Washington University School of Medicine have identified a variant of the brain protein aquaporin-4 (AQP4) as a potential target. Occasionally, a gene sequence may be mis-read into an adjacent gene, producing a longer protein than normal — a process referred to as extended read-through. Extended read-through of the AQP4 gene produces a long form of the protein in the astrocytes that help form the blood brain barrier. The researchers believe this long-form of AQP4 may help keep the brain free of unwanted proteins by helping to flush wastes such as Aβ into the blood stream. The researchers have also identified several initial compounds, including apigenin – a protein found in chamomile, parsley, onions, and other plants — that increase the production of long-form aquaporin-4 and appear to stimulate faster clearance of amyloid compared to placebo from the brains of treated mice.
In further global research pertaining to amyloid plaque build-up and cellular waste clearance, researchers at Hong Kong University of Science and Technology and a team of international collaborators have also identified a blood protein, soluble ST2 (SST2). High levels of this protein, built up during the aging process, can disrupt amyloid clearance by microglia. Thus, treatments aimed at down-regulating SST2 could open up new avenues for plaque clearance. Similarly, New York University researchers have identified flaws in the handling of cellular wastes associated with intracellular lysosomes that may be sources of plaque origination and targets for drug discovery. Each of these new findings and more add to growing evidence that issues that harm cellular waste management may be key signs of early AD, and that this emerging field of research offers broad potential for AD drug discovery.