
Since the emergence of the COVID-19 pandemic, it has become apparent that the virus can affect infected individuals in strikingly different ways. Some show no symptoms, but still spread the infection. Many have mild symptoms and quickly recover. But about one-fifth of infected individuals end up with severe disease that requires hospitalization, oxygen therapy, or mechanical ventilation, and may end in death. Even some of those who first present with mild-to-moderate symptoms may progress to more severe disease or may have illness that lingers for many weeks. As a result, there is an urgent need for effective biomarkers to help classify patients based on risk, so that aggressive monitoring and appropriate therapy can be promptly directed to individuals more likely to progress to more severe illness.
Until now, disease risk from COVID-19 has been determined primarily on a patient’s age and the existence of underlying medical conditions such as an immunocompromised state, obesity or heart disease. Research teams in China, Europe and the United States have been working diligently to identify blood-based biomarkers with the potential to pinpoint severe cases before they develop.
Early this year, a Chinese team identified 93 proteins and 204 metabolites whose blood levels correlate with severe disease. Using 29 of these markers, they trained a machine learning model to stratify patients by disease risk. The model was shown to correctly classify 29/31 patients in the training cohort, and 23/29 in two independent test cohorts. European researchers have also found 27 potential biomarkers that were expressed differently in hospitalized patients depending on the severity of the patient’s infection.
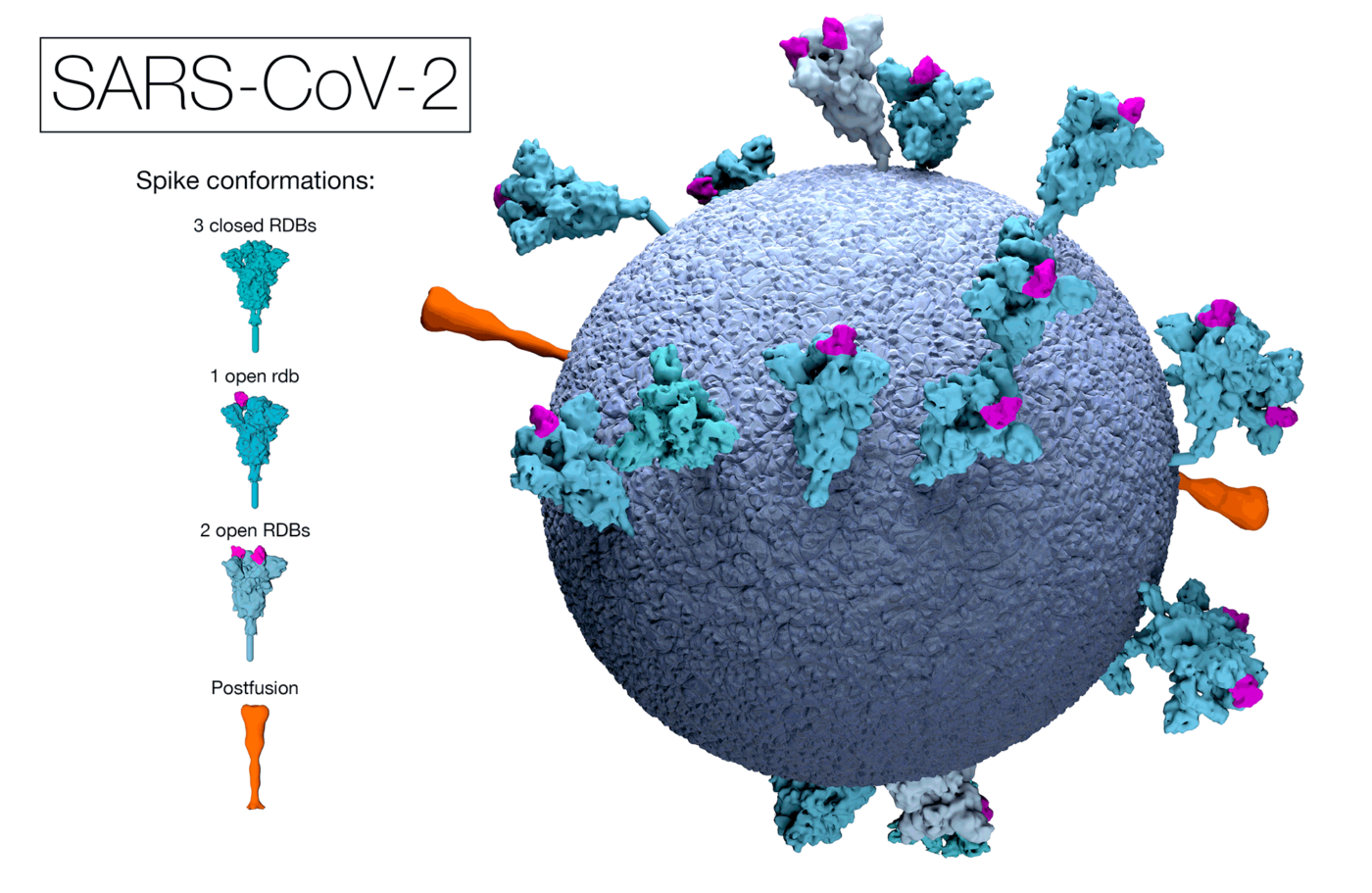
More recently, researchers from Harvard Medical School and the University of Washington have documented a set of immune biomarkers to classify patients according to likelihood of surviving COVID-19. The researchers used samples from a cohort of 22 patients, 12 of whom recovered and 10 of whom died. They employed a systems serology technique that used more than 60 assays to create a detailed profile of each patient’s immune response and found that patients who recovered had a humoral immune response primarily to the SARS-CoV-2 virus spike protein (S). In contrast, those who died had a stronger response to the N (nucleocapsid) protein that provides no protection against coronaviruses related to SARS-CoV-2. They showed that the dominance of the immune response – S versus N – was more predictive of patient recovery or death than demographic factors like patient sex or age.
A team at George Washington University has also reported five biomarkers in blood to be associated with higher levels of clinical deterioration and death: IL-6, D-dimer (related to blood clots), CRP (a marker of inflammation or infection), LDH (related to tissue damage), and ferritin (a mediator of immune dysregulation). Elevated levels of these markers are associated with inflammation and bleeding disorders, leading to increased risk of ICU admission. The highest risk of death occurred when LDH was over 1200 units/l and D-dimer was over 3 micrograms/ml. Similarly, a U.S.-China team has been developing a model that predicts risk based on levels of D-dimer, CRP, and procalcitonin (associated with infection and sepsis). Each marker was relevant to COVID-19 complications and dramatically increased in patients that died. The model ranked patient risk on a level between 0-100, with the higher score correlating to higher risk of death.
The “holy grail” for many COVID-19 teams has been the identification of biomarkers that might quickly spot patients with apparently mild symptoms who are on track to develop the intense immune response that results in severe disease, so that appropriate interventions can be directed appropriately. Researchers at Yale University performed longitudinal analyses of various types of white cells and blood-based markers in 113 hospitalized COVID-19 patients with moderate or severe disease, and a similar number of healthy individuals who served as controls. They found that several specific cytokines were increased in infected patients than in healthy controls, providing a ‘core’ signal of COVID-19 infection. Other specific sets of cytokines and molecules associated with blood clotting abnormalities were found to distinguish patients with severe disease from those moderately affected. Additionally, at early time points after infection was diagnosed, patients progressing to moderate disease could be distinguished by low levels of inflammatory markers and rising levels of proteins associated with tissue repair. In contrast, those who progressed to severe disease had increased levels of several inflammatory markers even early in their infection. The researchers are now looking at patients with very early signs of infection to see if there are differences in markers between individuals who ultimately do and do not require hospitalization. If people at high risk of more severe disease could be identified early, it might be possible to treat them with therapies that limit viral replication, with the goal of reducing the need for hospitalization.