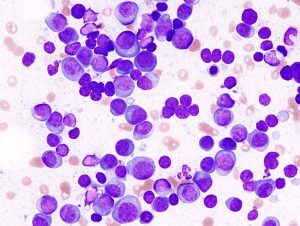
 Multiple myeloma (MM) is a deadly bone marrow cancer. In recent years, the treatment landscape for this disease has improved considerably. However, most patients still relapse and the need for new and better therapeutic options endures.
Multiple myeloma (MM) is a deadly bone marrow cancer. In recent years, the treatment landscape for this disease has improved considerably. However, most patients still relapse and the need for new and better therapeutic options endures.
Encouraging news about several approaches were reported at the American Society of Hematology (ASH) in December. Results from a Phase 3 trial combining Johnson & Johnson’s Darzalex (daratumumab) with the commonly used MM drugs Revlimid (lenalidomide) and the immunosuppressant dexamethasone reduced the risk of death for newly diagnosed patients not eligible for bone marrow transplant by 44% — an achievement that some experts were hailing as a new standard of care.
The latest approach to treating MM, however, centers on the use of chimeric antigen receptor T-cell (CAR-T) therapies that target B-cell maturation antigen (BCMA). Several groups who are developing BCMA-CAR-T therapeutics, including Bluebird/Celgene, Nanjing Legend Biotech/Johnson & Johnson, and Poseida Therapeutics, reported encouraging Phase 1 and 2 data in heavily pretreated patients. Each study resulted in very high overall rates of response as well as sizeable numbers of complete responses. However, questions remain about the durability of the responses, and serious cases of cytokine release syndrome, a potentially fatal adverse event that has plagued CAR-T therapies, remain a risk. Bluebird/Celgene has now enrolled a pivotal study (KarMMA) of BB2121, its CAR-T therapeutic, and hopes to file for approval in 2020; Poseida expects to begin a pivotal trial in 2019 and file for approval by the end of 2020. A variety of other companies in both the United States and China are developing further BCMA-CAR-T treatments.
Further potential competition amongst BCMA-targeting agents has emerged in the form of bi-specific antibodies that simultaneously bind and bring together T-cells (targeting the CD3 antigen on their surface) with cancer cells expressing BCMA. Amgen presented data from a Phase 1 dose-ranging study of AMG420, its BCMA bi-specific antibody, which is administered via a four-week continuous infusion. Of the 10 heavily pretreated patients receiving a 440 μg/day dose, seven responded — and six were still responding after 7.5 months. Four patients had complete responses with no residual malignant cells in their bone marrow. However, while no patients receiving lower doses of AMG420 (up to 400 μg/day) had significant adverse events, several patients treated at higher doses experienced infections and one developed a serious peripheral neuropathy. Amgen is also developing a follow-on version of the bi-specific antibody with a longer half-life, which the company hopes will reduce the inconvenience of the drug’s administration compared to AMG420
Bi-specific antibodies are also under development for the treatment of relapsed B-cell lymphoma. Regeneron presented data on a CD20-targeted bispecific antibody (CD20xCD3), which achieved an 80% complete response rate in a small study of a once-weekly treatment in heavily pretreated patients with follicular lymphoma. The company expects to conduct a pivotal study of this antibody in 2019. Regeneron is also developing other bi-specific antibodies, including a BCMA-targeting treatment for MM that will enter clinical trials during 2019, and one targeting MUC16 for the treatment of ovarian cancer, currently in early stage clinical trials.
It’s too early to say whether bi-specific antibodies will pose serious competition to CAR-T therapeutics, as they are earlier in development and there is not yet much data on the durability of patient response. As off-the-shelf treatments that can be provided immediately, bi-specific antibodies offer some advantages over the four-week wait for CAR-Ts, which must be generated individually for each patient. Furthermore, relatively few treatment centers can currently provide CAR-T therapies. Bi-specifics are also likely to be less expensive. However, response rates to date for bi-specific antibodies have been slightly lower than those seen for CAR-T treatments (at least in MM), and bi-specific antibodies have also been associated with some serious adverse events.